Stomach Pathology Part 1
this post will contain the following:
Now we will talk about the Chronic gastritis, the symptoms here are less severe , more persistent, without EROSIONS and no HEMORRHAGE, the causes of Chronic gastritis are a lot, we have chronic infection by H. pylori being the most common. Other causes include autoimmune gastritis (atrophic gastritis), alcohol and cigarette smoking, postsurgical reflux of bile, and radiation exposure. Additionally, motor and mechanical issues such as obstruction, bezoars (luminal concretions), and gastric atony can contribute to the condition. Granulomatous conditions, like Crohn’s disease, can also lead to chronic gastritis.
NORMAL: Anatomy and histology of the stomach
PATHOLOGY:
1-CONGENITAL
2- GASTRITIS
part 2 will contain:
3-PEPTIC ULCER
4-TUMORS
Anatomy:
starting with the normal anatomy of the stomach, the stomach is divided into anatomic regions, the Cardia, the funds, the body and the antrum and end with pylorus as u cab see in the picture:
Cardia: This is the area where the esophagus connects to the stomach. It’s the entry point for food. it is also lined by mucin-secreting cells with shallow glands.
Fundus: This is the upper portion of the stomach, above the cardia. It’s where gas tends to accumulate.
Body (Corpus): This is the main central region of the stomach where most of the food is mixed with digestive juices. both
The body and fundus: have Well-developed glands contain chief cells that produce and secrete digestive enzymes such as pepsin.
Antrum: This is the lower part of the stomach that helps grind up food and mix it with digestive enzymes. It also regulates the passage of food into the duodenum. it also has the antral glands,t he antral glands similar but contain endocrine cells, (G cells, release gastrin)
Pylorus: This is the opening at the end of the stomach that leads to the small intestine. It controls the release of partially digested food into the duodenum.
the stomach is supplied with the celiac trunk mainly and for the veins it drains into the portal vein.
Histology:
the stomach has a lot of types of cells in its wall, it has the surface Mucus cells which produce mucus MAINLY, we also have the parietal cells which produce HCL, and they are important as they produce intrinsic factor essential for the absorption of B12, so any disease that can affect these cells will cause malabsorption of B12. we also have Chief cells which produce pepsinogen and gastric lipase and finally the G cells which secrete a very important hormone which is gastrin.
INFLAMMATORY DISEASE OF THE STOMACH
Gastritis: inflammation of mucosa it is Often generalized.
Erosion: loss of epithelial layer
which can Extend into muscularis mucosa
• If they break through it will cause the formation of an ulcer, which can extend into the deep layers of the wall of the stomach, these ulcers are usually focal in shape, and it mostly occur in the duodenum and the stomach cause of the acid accumulation.
The gastritis can be, acute, chronic or Autoimmune. starting which the ACUTE GASTRISITS, the acute gastritis is usually transient, short and superficial, but in some in more severe cases there may be mucosal erosion, ulceration, hemorrhage, hematemesis, melena. there are punch of causes that may lead to acute gastritis such as, Alcohol consumption, heavy smoking, ischemia and physical trauma and using NSAIDS. HOW?
NSAIDs
• Block prostaglandin production
• Increase acid production
• PGs also promote mucous/bicarb production
• Common in chronic NSAID users
• Alcohol
• Damages mucosa
• Chemotherapy
• Inhibits epithelial cell replication
• H. Pylori (bacterial infection)
Histological picture of Acute gastritis: Acute erosive hemorrhagic gastritis: Erosion +Hemorrhage also may occur,manifesting as dark puncta in an otherwise hyperemic mucosa with neutrophils.
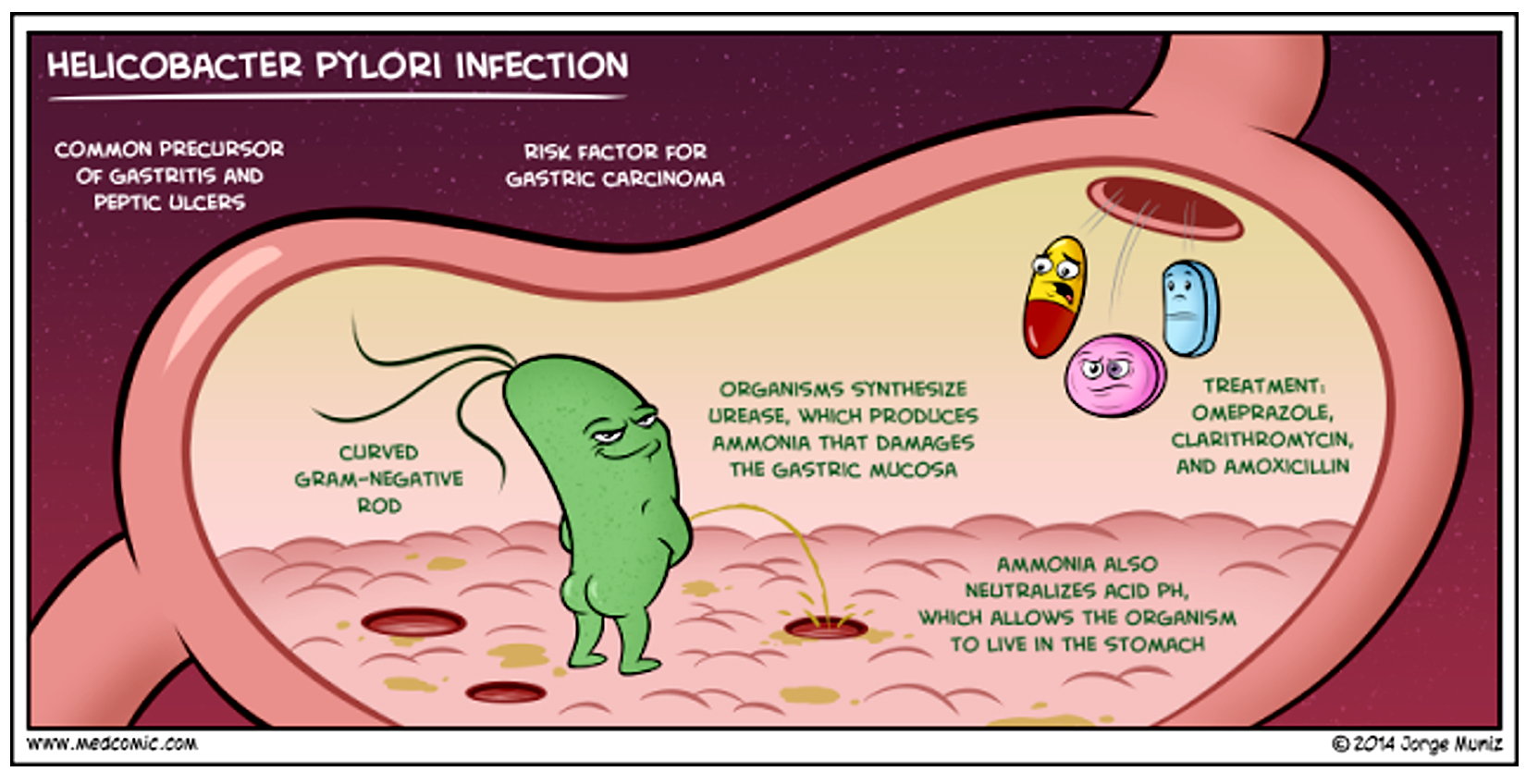
starting with H pylori, Helicobacter pylori (H. pylori) is the leading cause of both acute and chronic gastritis, affecting the stomach’s antrum. It increases acid secretion, contributing to conditions like peptic ulcers. The bacteria produce harmful factors, including ureases, proteases, and vacuolating cytotoxin A (VacA), which damage epithelial cells, disrupt cell junctions, and cause cell death. Additionally, CagA, a key protein, triggers the production of IL-8, which boosts inflammation and promotes cell growth while inhibiting apoptosis. This leads to dysplasia and can increase the risk of gastric cancer. H. pylori's virulence is due to its flagella (helping it move through mucus), urease (which protects it by neutralizing stomach acid), adhesins (helping it stick to cells), and toxins (which damage cells). This inflammation can lead to the formation of non-neoplastic inflammatory polyps.
Now to the autoimmune type, Autoimmune gastritis is characterized by the destruction of parietal cells, primarily found in the body and fundus of the stomach. This process is T cell-mediated, making it a Type 4 hypersensitivity reaction. The immune system attacks either the parietal cells or intrinsic factor (IF), leading to mucosal atrophy and a decrease in acid production, known as achlorhydria. As a result, gastrin levels increase since the usual negative feedback mechanism from acid is lost. The G cells in the antrum, which produce gastrin, undergo hypertrophy in response. This condition also causes pernicious anemia due to the antibodies destroying intrinsic factor, preventing the absorption of vitamin B12 in the terminal ileum. Vitamin B12 deficiency can lead to peripheral neuropathy. Furthermore, autoimmune gastritis increases the risk of gastric adenocarcinoma as chronic inflammation leads to intestinal metaplasia, which is driven by inflammatory infiltrates and lymphocyte signaling.
here is a good summary:
that is it for part 1 see uuu in part 2.
stay safe




Comments
Post a Comment