Biochemical aspects of gastric secretion
In this post we are going to discuss the following:
1 - the properties of the gastric secretion.
2- the tests used in diagnosing some gastric related disorders.
Starting with the main constituents of the Gastric secretion:
1- HCL-Secreted by Parietal cells
2- Pepsinogen- Secreted by Chief cells
3- Intrinsic factors- Secreted by Parietal cells and it is Required for B12 absorption.
4-Alkaline Mucous-Secreted by Mucus cells coat the gastric cells and acts as a lubricant
For more information about these constituents refer to the Gastric secretion physiology post form here
What are the gastric secretion properties?
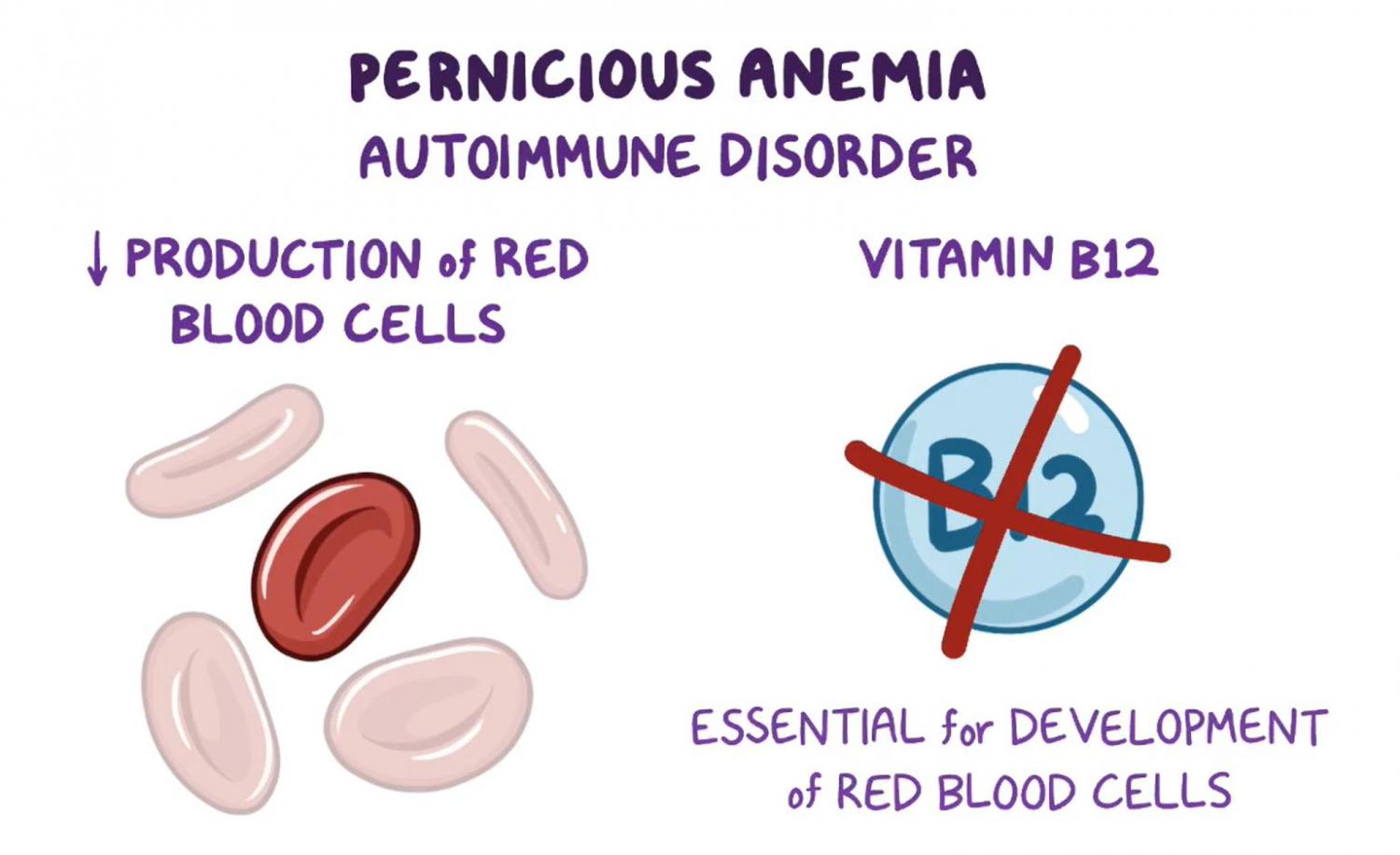
Gastric secretion typically has a volume of 20-50 ml and appears colorless to pale yellow. The pH of the secretion ranges from 1.6 to 4.8, making it acidic. Free HCL content is between 0-40 mmol/l, while total acidity falls between 10-50 mmol/l. Pepsin, mucin, and intrinsic factor (IF) are all present in gastric secretion. Bile might also be present as a normal component of the gastric secretion. Hyposecretion of gastric juice can occur in conditions such as pernicious anemia, extensive carcinoma of the stomach, and chronic gastritis. In these cases, gastrin levels are expected to rise because reduced acid secretion causes the loss of the negative feedback inhibition.
Now for the next part and the important one is the tests used in diagnosing some gastric related disorders. what are these conditions?
1-Gastro-esophageal reflux diseases (GERD)
2- peptic ulcer diseases
3- Vitamin B12 deficiency
4-Gastrinomas (Zollinger Ellison Syndrome)
5-effectiveness of vagotomy
Starting with Gastro-esophageal reflux diseases (GERD):
first of all, what is GERD? a condition where there is a Backflow of acid and stomach content into Esophagus. GERD occurs when stomach acid frequently flows back into the tube connecting mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of esophagus.
what are the tests used for this disease?
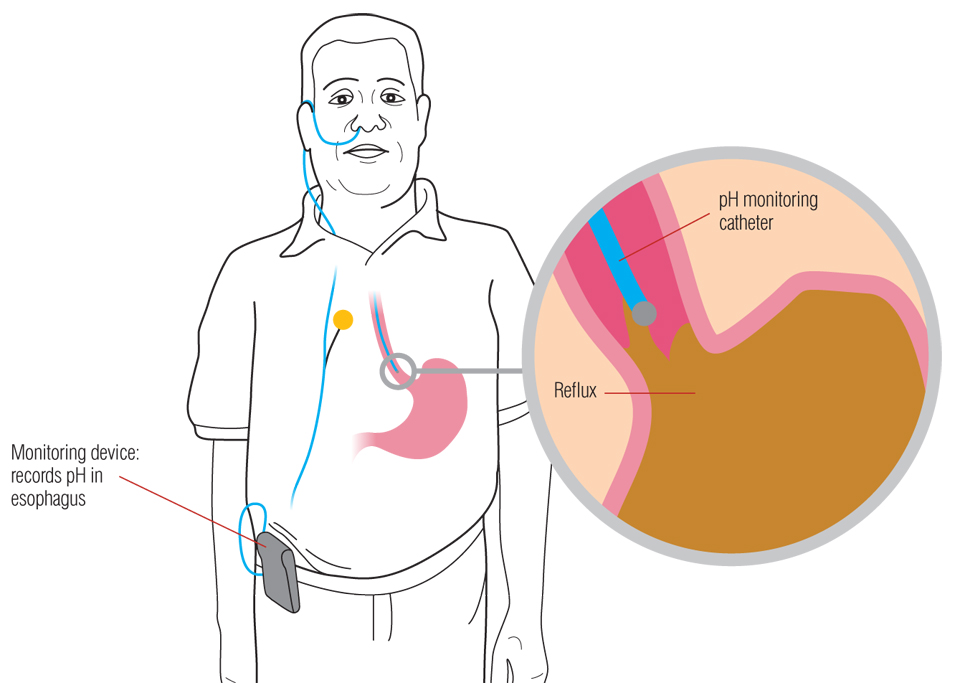
1- PH monitoring using either Naso-esophageal catheter that has an acid sensitive Tip or Wireless PH testing, A naso-oesophageal catheter with an acid-sensitive tip is inserted during fasting. The catheter remains in the nose for 24 hours while the patient continues their normal daily routine. Preparations include fasting for 4-6 hours before the appointment and discontinuing proton pump inhibitors, H2 blockers, and antacids prior to the procedure. and for the Advanced method for pH measuring is the Wireless pH Testing (radiotelemetry pH sensing capsule to the mucosa of the distal esophagus,
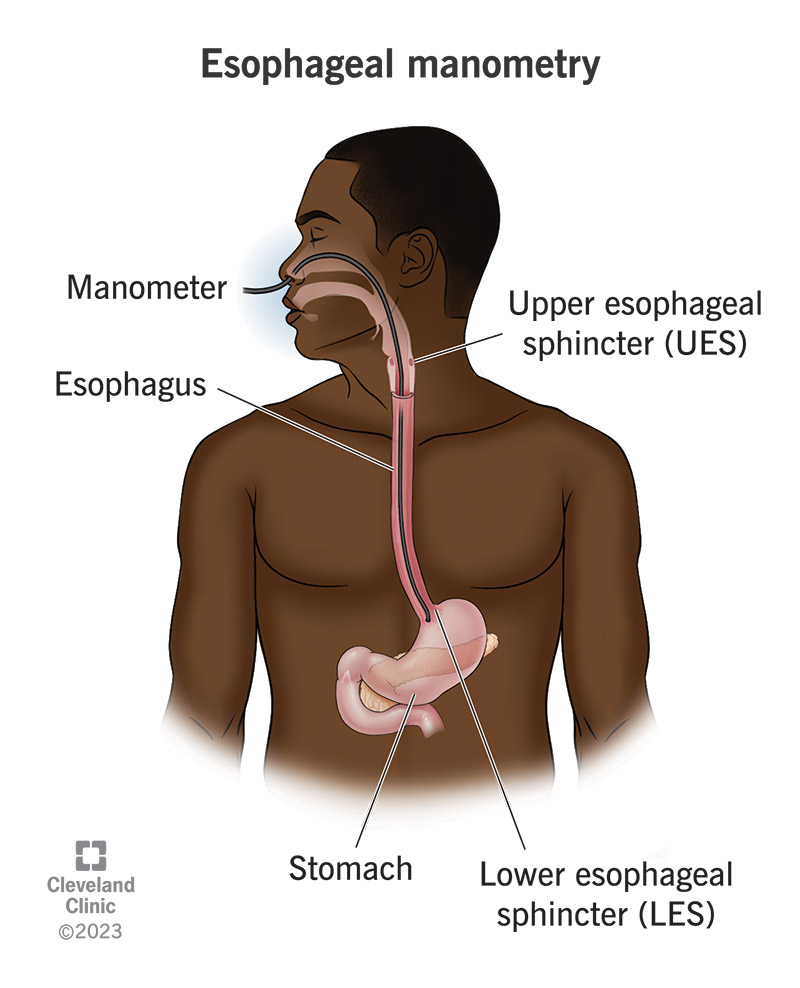
and lastly we have the manometry, Manometry is a diagnostic procedure used to measure pressure t the gastrointestinal tract and esophagus. Manometry evaluates muscle and sphincter function, helping in
diagnosing motility disorders and assessing lower esophageal sphincter (LES) pressure for surgical planning.
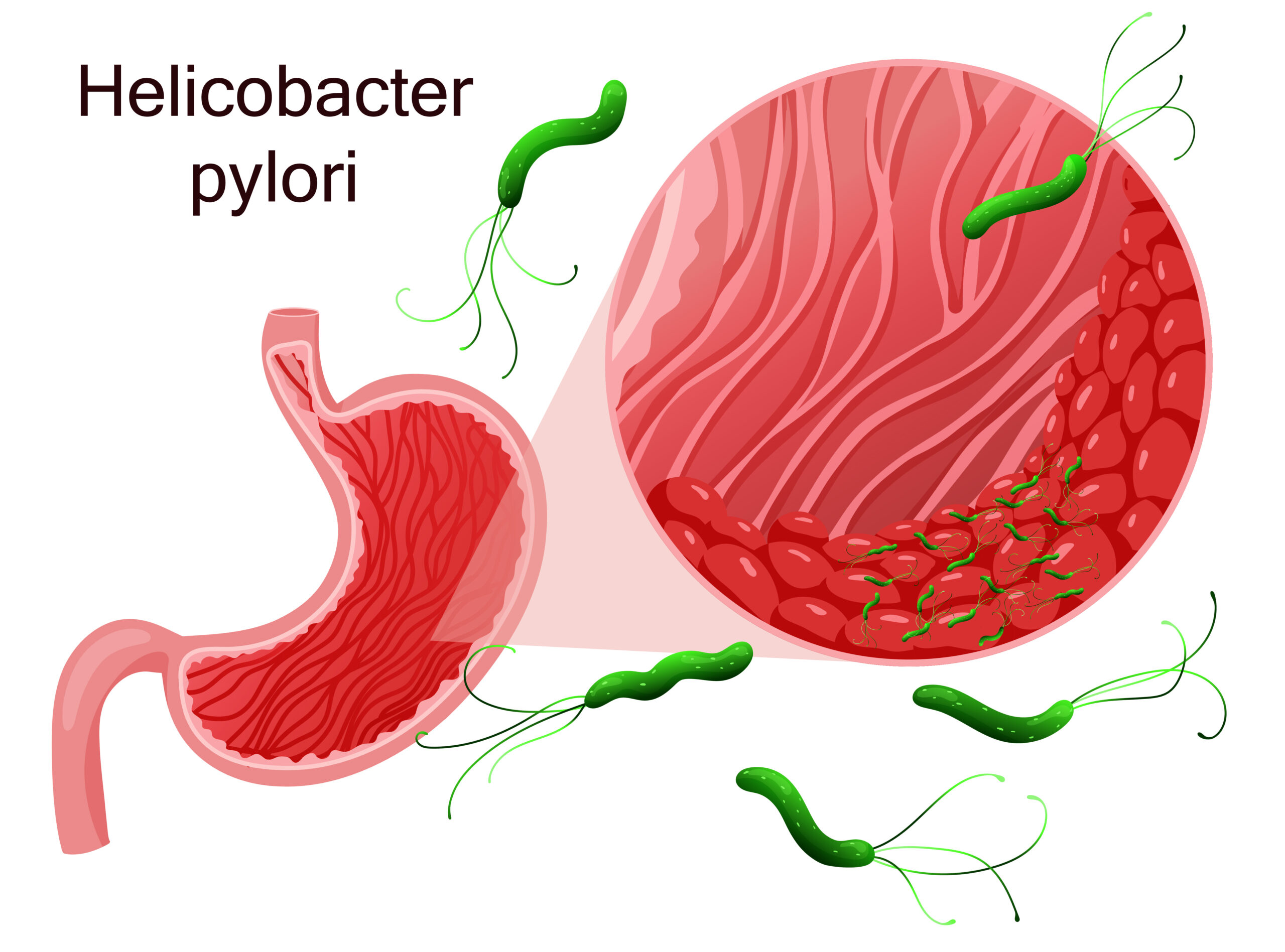
Now with the Peptic ulcers, A peptic ulcer is an open sore that forms on the lining of the stomach, small intestine, or esophagus. When it occurs in the stomach, it is referred to as a gastric ulcer. A duodenal ulcer is a type of peptic ulcer that develops in the initial part of the small intestine, known as the duodenum. in this disease we usually start by detecting one of the most common causes of peptic ulcers, which is a microorganism called Pylori, we are going to talk about it in a separate post, but for now the important thing to know is that this bacteria can produce an enzyme called UREASE, this enzyme can convert the Urea to CO2 and Ammonia, this ammonia that is being produced can neutralize the acidity of the stomach acid, making this bacteria able to live in the acid environment of the stomach, and because it neutralize the acid, this will stimulate the Parietal cells that we already talked about in the pathology post , produce more HCL and damage the mucosal cells even more .
For the tests that can be used to detect this Microorganism, first of all we have Urea breathing. Patients
are given C13 (Carbon isotope) labelled urea with a fruit drink or a capsule. The breath sample is taken after 30 minutes. High concentration of labelled C13 in CO2 indicates the presence of H. pylori in gastric mucosa, in short if the bacteria is there and we gave it a urea with a labelled CO2 after the patient exhale, if there are a high concentration of the labelled CO2 this means the test is positive, for more information i recommend u to see this video:
are given C13 (Carbon isotope) labelled urea with a fruit drink or a capsule. The breath sample is taken after 30 minutes. High concentration of labelled C13 in CO2 indicates the presence of H. pylori in gastric mucosa, in short if the bacteria is there and we gave it a urea with a labelled CO2 after the patient exhale, if there are a high concentration of the labelled CO2 this means the test is positive, for more information i recommend u to see this video:
this is a photo to help u understand:
we also have other ways such as: Serological Helicobacter pylori IgG antibody: This enzyme-linked immunosorbent assay (ELISA), detects IgG antibodies to H. pylori and Faecal Helicobacter pylori antigen. and there are also some invasive procedures, that include taking a biopsy like the Rapid Urease test, which include taking the biopsy and adding urea and if H pylori is present it will hydrolyse the urea prod ammonia and changing pH.
Now with Gastronomas :
Zollinger Ellison Syndrome involves Gastrin-secreting neoplasm- located in pancreatic islets
In this syndrome there is very high secretion of Gastrin (60% more) compared to a basal secretion.
Gastrin stimulates HCl secretion causing ulcers.
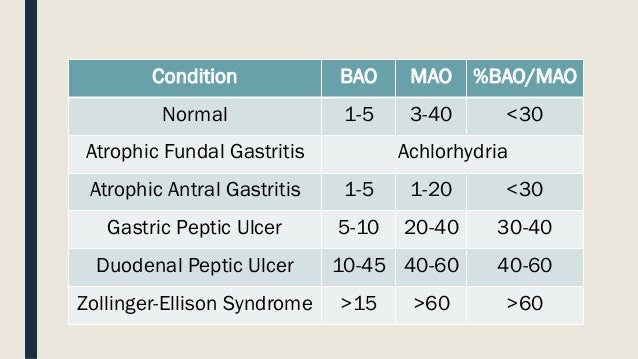
So, measurement of gastrin is very important to confirm or diagnose such diseases, affects stomach, excessive secretion and makes the ulceration and damage of stomach walls. Levels of gastric acid secretion differ in various disease states and their measurement may help in the diagnosis and treatment of these diseases, High levels of acidity are seen in duodenal ulcers and patients with Zollinger–Ellison syndrome. There are 2 tests can measure both basal and stimulated acid secretion Two types of Gastric Acid Output
Basal Gastric Acid Output (BAO)
Post stimulation (maximum acid output-MAO)
starting with: Measuring Gastric Acid Basal Acid Output (BAO)
Basal acid output (BAO) refers to the amount of stomach acid produced when the stomach is empty and not being stimulated by food or other factors. BAO levels can vary throughout the day, even from hour to hour. To measure BAO, gastric acid is collected by suctioning it from the stomach over a one-hour period, typically divided into four 15-minute samples.
for the Post stimulation (maximum acid output-MAO)
To measure stimulated gastric acid output, the process starts similarly to the basal acid output measurement. The patient fasts and is then intubated. Following this, a dose of synthetic pentagastrin (6 mg/kg, administered subcutaneously) is given. Pentagastrin is a synthetic peptide that mimics natural gastrin, which stimulates the production of stomach acid, pepsin, and intrinsic factor. After the injection, gastric secretions are collected every 15 minutes for an hour, just like in the basal output test. The collected samples are then analyzed by measuring the volume, pH, and acidity (via titration), and the total acidity is calculated for both the basal and stimulated samples. This method helps assess how the stomach responds to stimulation with pentagastrin.
so, In the case of Zollinger-Ellison syndrome, the results of acid output measurements are significantly higher than normal. For Basal Acid Output (BAO), it would be greater than 20 mEq/hour, indicating that the stomach is producing much more acid than usual. When the stomach is maximally stimulated, the acid output can exceed 60 mEq/hour, far surpassing typical levels. This is due to the presence of tumors (gastrinomas) that produce excessive amounts of gastrin, which in turn causes the stomach to overproduce acid. see the picture below to know the normal values and other values for other diseases
Intrinsic factor (IF) is a glycoprotein secreted by the parietal cells of the stomach. It is essential for the absorption of vitamin B12 in the terminal ileum.When the parietal cells in the stomach are damaged, like in pernicious anemia, they can’t produce intrinsic factor (IF), which is needed to absorb vitamin B12. This can happen due to autoimmune issues, stomach surgery, or certain rare genetic disorders. Without IF, B12 absorption is blocked, affecting blood and metabolism. Often, the problem lies in absorption itself, with antibodies causing issues. Helicobacter pylori infections can also lead to atrophic gastritis, further damaging the stomach and hindering IF production.
there are two types of antibodies for the intrinsic factors, one type that will block the intrinsic factor receptor for V12 and so Vitamin b12 will not be taken by the intrinsic factors, the other type is called binding antibodies, which will bind to the intrinsic factor-V B12 COMPLEX and stop it from binding to its binding sites in the intestine.
Lastly, we have the Vagotomy:
vagotomy is a surgical operation in which one or more branches of the vagus nerve are cut, typically to reduce the rate of gastric secretion (e.g. in treating peptic ulcers).
and we can test if the surgery has done its work or not by a test called Post-vagotomy insulin test
, in this test we will give the patient insulin, which will cause hypoglycemia, in normal cause hypoglycemia will stimulate the vagus nerve causing increased secretion of HCL, so if the Vagotomy was successful we won't see any production of HCL.
For any questions u can always reach us by our email or in the comments section.
stay safe until the next time

Comments
Post a Comment